Quality initiatives
We're dedicated to providing you the care and service you deserve. Our quality initiatives ensure we understand, prioritize, and meet our members' needs.
Quality Improvement Program
- Improve member care, service, experience, access and/or safety; and/or
- Improve service to practitioners, providers, employers, brokers and other customers and partners; and/or
- Improve Medica's internal operations related to care, service, experience, access and patient safety.
The QI program supports Medica's mission to be the trusted health plan of choice for customers, members, partners and our employees.
Our QI program covers a wide range of topics that affect our members, providers, employers and brokers, as well as our internal staff. We want to be sure that:
- Our members receive high-quality health care and service from our providers.
- Our members can get appointments quickly. We have enough doctors in the areas where our members live.
- Our members get the help they need when they change doctors.
- Our complaint and appeal processes work fairly and efficiently.
- We can offer appropriate help to our members with chronic health problems.
- We can help our members be sure that the care they receive is safe.
- Our members are satisfied with Medica, and we're identifying areas where we can do better.
To create an effective quality plan, Medica must understand what our customers need, want and believe about health care. We learn about members and other important stakeholders through satisfaction surveys, reports on member complaints and appeals, focus groups, market research and other data that shows the kind of care our members receive and how well it works for them.
Medica evaluates the QI program at the end of each year. The Quality Improvement Program Evaluation is a report that reviews how well we did on our quality improvement activities. In the report, we compare measurements and look for trends to see how well we've done over time. If we didn't meet a goal, we also report on any problems or unexpected happenings that kept us from being successful.
The QI Program Evaluation is an important learning tool for Medica. The information in the report helps us understand how effective our QI program has been, and also helps us make recommendations for the next year's work plan.
When Medica chooses QI projects, we look for the best opportunities to improve care, service and safety for the greatest number of members. These are some of the questions we consider:
- Will this improvement be meaningful to our members?
- Do we have the ability to make a real impact on the problem?
- How are we doing compared to other local and national health plans? Can we do even better?
- What laws and regulations do we need to consider?
- What will it cost – in dollars, time, and staff – to do this project well?
Once we choose a project, we set a performance goal. We measure progress toward the goal throughout the project to see how effective the improvement is.
Every year, Medica prepares a Quality Improvement Work Plan. The work plan is a summary of the key QI activities we plan for the year. Here are some examples of projects on the current work plan:
Every work plan activity has an "owner" — a Medica staff member who watches over the project and reports on progress. Some projects or goals may change during the year if progress reports show we aren't getting the results we need. We may also add new projects throughout the year.
Medica evaluates the QI program at the end of each year. The Quality Improvement Program Evaluation is a report that reviews how well we did on our quality improvement activities. In the report, we compare measurements and look for trends to see how well we've done over time. If we didn't meet a goal, we also report on any problems or unexpected happenings that kept us from being successful.
The QI Program Evaluation is an important learning tool for Medica. The information in the report helps us understand how effective our QI program has been, and also helps us make recommendations for the next year's work plan.
At Medica, quality is everyone's responsibility. Departments and staff throughout Medica "own" and participate in QI activities. The Senior Medical Director, a licensed physician, is responsible for leading the QI program. Staff in the Quality Improvement department monitor and support program activities.
Medica's Quality Improvement Subcommittee (QIS) directs and oversees the QI program. QIS is staffed by Medica employees representing key business units across the organization. QIS reports to the Medical Committee of the Medica Board of Directors. The Medical Committee then reports to the full Medica Board of Directors.
For more information
We always welcome member feedback! If you'd like to share your comments or suggestions, or would like more information about Medica's QI Program, please contact our Customer Service Department at 952-945-8000 or 1-800-992-3455 available from 9 a.m. – 5 p.m. CT, Monday – Friday.
Medicaid Quality Improvement Program
Medica has Quality Improvement (QI) activities focused on improving health outcomes for our Medicaid members. We offer Medicaid plans across Minnesota for all ages and abilities. They include:
- Plans for people age 65 and older: Minnesota Senior Health Options (MSHO) and Minnesota Senior Care Plus (MSC+)
- Plans for people age 18-64 with disabilities: (Special Needs BasicCare (SNBC) and Special Needs BasicCare with Medicare (Integrated SNBC or ISNBC)
- Plans for people age 0-64: Prepaid Medical Assistance (PMAP) and MinnesotaCare (MNCare).
We understand that the needs of our Medicaid members vary. That is why each year we identify QI activities aimed to improve the health of our members. Current focus areas include:
- Reducing disparities in health outcomes. This includes special focus on diabetes care and care for pregnant members, infants, and children.
- Community Engagement Activities
- Improving oral health outcomes and access to dental care
Examples of QI activities in these focus areas include:
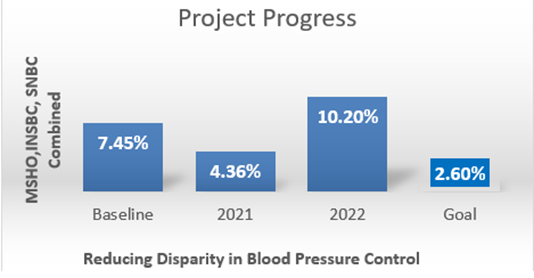
- Medica worked with other Minnesota Health Plans on a 3-year Performance Improvement Project (PIP). The project aimed to improve diabetes care and decrease the disparity in blood pressure rates between Black, Indigenous, and People of Color (BIPOC) members and non- Hispanic White members.
- The PIP ran from 1/1/21 through 12/31/23. The project focused on members enrolled in our MSHO, MSC+ and SNBC products.
- To measure the success of the PIP, we are using a measure that looks at the percentage of members with diabetes whose blood pressure is considered well-controlled (<140/90 mm Hg).
- When we measured the disparity in blood pressure control before starting the project, we found a disparity of 7.45%. BIPOC members were less likely to have well-controlled blood pressure compared to non- Hispanic White members.
- Our goal is to decrease that disparity to 2.60% over the course of the project.
- In 2022, blood pressure control improved for all groups. This is a good sign. It tells us that more members are working with their doctor to manage their blood pressure.
- The increase in rates also increased the disparity gap. Although more BIPOC members are managing their blood pressure well, they are not improving at the same rate as the non-Hispanic White members.
- Based on the 2022 results, we did some targeted outreach to members to educate them about diabetes resources available to them.
- Lessons Learned: While we are making progress toward our goal, disparities remain in certain populations. Also, members don’t always know about the benefits and incentives available to them that could help them manage their diabetes better.
- Next Steps: This project ended 12/31/23. We will have final results later in the year. Many of the interventions for this Diabetes PIP are continuing in a new PIP that started 1/1/24. The new PIP focuses on diabetes and depression. See below for more detail on the new project.
- Medica continues working with members and providers on ways to improve diabetes health and address the social and environmental factors that impact health. This includes providing targeted education to Care Coordinators, so they have information to help members manage their diabetes. In addition, our pharmacy team and Disease Management nurses continues to outreach to members to provide education and address barriers members may be experiencing. Medica also continues to offer several benefits and incentives to support members with their diabetes care and management, including gym memberships, nutrition programs, foot care, and others. We work to increase the use of these benefits and incentives by providing more education to both members and their Care Coordinators.
Visit here for helpful resources on diabetes: Diabetes - MyHealthfinder | health.gov
- This new project is in effect from 2024 through 2026 and focuses on improving care for MSHO, MSC+ and SNBC members who experience both diabetes and depression.
- Diabetes and depression are both top conditions within Medica’s Senior and SNBC populations.
- Medica chose to focus on a measure of kidney health for this project. It looks at whether members are being screened at least once a year to see if their diabetes is having an impact on their kidneys.
- The goal is to increase the number of members with diabetes and depression who are receiving kidney health screenings by the end of the three-year project.
- We also will monitor for disparities in screening rates. Our baseline data from 2022 showed that BIPOC members have better screening rates than non-Hispanic White members, but overall rates are low.
- Next Steps: Implementation of this project is in full swing. The year started with a phone call campaign to MSHO and ISNBC members to make sure they are aware of benefits that can help them manage their health.
- Medica is committed to improving maternal and early childhood health outcomes for our Medicaid members. In 2024, we are continuing our Healthy Start Performance Improvement Project (PIP) where we partner with other Minnesota health plans to improve care and health outcomes for expectant mothers and children enrolled in our Prepaid Medical Assistance Program (PMAP) and MinnesotaCare (MNCare) plans.
- One goal of this PIP is to better understand what our members feel is most important to them when it comes to maternal and early childhood health. To accomplish this, we are hosting member advisory meetings during the lifecycle of this project. Other goals include building relationships with community partners, developing educational webinars and tools, increasing engagement in our pregnancy programs, and increasing the use of doula services. Success will be measured by increasing timely prenatal and postpartum visits.
- Medica’s Pregnancy Programs offer personal support, guidance, and information throughout a members’ pregnancy. We also provide maternity Community Health Workers (CHW) to support pregnant women who may have socioeconomic risk.
- Members also can earn rewards for receiving prenatal and postpartum services, as well as for completing well-child visits and vaccinations. To see the full list of services that qualify for rewards, click here: Rewards and Incentives
- Lessons Learned: We have found that members are not always aware of the benefits available to them related to maternal and early childhood health. We have an opportunity to promote our pregnancy programs more effectively and to increase engagement.
- Next Steps: Since Medica expanded our service area to an additional eighteen counties in 2023, we are continuing to learn about our growing membership. We are closely monitoring prenatal and postpartum care rates to identify opportunities to increase engagement and the effectiveness of our pregnancy programs.
- To learn more about Medica’s pregnancy program, click here: Medica Pregnancy Program
- We understand that oral health is an important part of overall health. Taking care of your mouth and teeth can help prevent both dental and medical problems. So, our goal is simple – to increase the number of members that visit the dentist each year.
- In 2023, Medica hosted metro and regional member advisory meetings to gain feedback from our members about their oral health care experiences and to understand the barriers that they have faced in getting the dental care they need.
- Medica has initiated innovative programs to connect with our Medicaid members. Last year, we partnered with a critical access dental provider to reach out to thousands of members to help them find a dental home and schedule a dental appointment.
- We are trying new ways to communicate and educate our members on the importance of receiving regular dental screenings – whether that be through a phone call with a licensed dental professional, SMS text, or e-mail.
- We also continue to partner with our Care Coordinators and provider partners to raise awareness of the oral health needs of our members.
- While we have not yet reached our annual dental visit goal for all Medicaid products, we have seen year-over-year improvement in some of our plans.
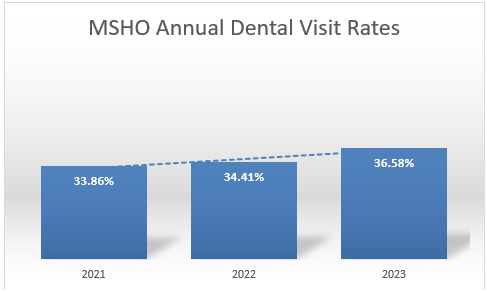
- Lessons Learned: Through community engagement events and member feedback, we have learned about how past dental experiences have significantly affected our members willingness to seek preventive dental care. Access and availability of dental providers that accept Medicaid continue to be a barrier to our members. We have also learned through our outreach program that our senior population prefers in-person care.
- Next Steps: Identify opportunities to educate members more effectively on the importance of oral health. Continue personalized outreach efforts to encourage preventive dental care and reduce the need for urgent or emergent dental procedures. Explore increasing incentives or rewards for members to improve annual dental visit rates.
- Medica values member feedback on their experiences with Medica and their health plan benefits.
- Medica hosts several Advisory Committee Meetings each year. The meetings provide a safe and welcoming environment for members, advocates, providers, county representatives and other key stakeholders to share their feedback, concerns, and ideas.
- The Advisory Committees are considered key partners for input on such things as health equity challenges and opportunities and benefit design.
- The Advisory Committees’ input is highly valued by Medica, and action is taken based on the groups’ input.
- Lessons Learned: Participation in member meetings has been lower than expected, but feedback from those that have participated has been overwhelmingly positive. Through our community engagement efforts, we identified that many participating members were unaware of the many value-added benefits offered by their health plan.
- Next Steps: We are exploring new meeting venues, locations, and meeting times to encourage greater participation in our member advisory meetings. We are actively tracking and trending our members’ input in an effort to tackle larger, organizational-level issues, such as plan benefit education. We have also learned from our members that their personal experiences with their healthcare providers have had a significant impact on their health and well-being.
Quality resources
Finding quality health care for yourself or your loved ones is often a primary — and sometimes puzzling — concern. We want to connect you with the information you need to make sound health care choices for yourself and your family.
Below you will find a variety of resources you can use to research the quality of care provided by physicians, primary care clinics and hospitals.
HealthGrades National Health Index: This site provides accessible and transparent information on physicians and hospitals as well as helps users connect with their provider of choice.
NCQA Health Care Report Card by Practice: These reports examine how well doctors, other clinicians, practices, health insurance plans and other health care organizations nationwide perform. The report cards are a compilation of all NCQA accreditation, recognition, certification and distinction programs.
Administrators in Medicine (AIM) DocFinder: This online physician directory contains licensing and disciplinary information of health care practitioners by state.
MN Community Measurement (MNCM): MNCM develops measures, collects data and creates reports that drive improvement in health care. Its mission is to accelerate health care improvement by public information reporting.
The Leapfrog Group: This national nonprofit collects and transparently reports and compares hospital performance based on their quality of care, giving consumers the information they need to make informed decisions.
MN Department of Health Adverse Events Search: Area hospitals are required to report to the MN Department of Health whenever any of 28 identified preventable adverse events occur.
Medicare.gov Hospital Compare: This tool allows you to compare hospitals based on their quality of care, patient survey results, rates of readmission, mortality rates and more.
Quality Check: This site lets you see whether a health care organization has been accredited or certified by the Joint Commission.
Nursing Home Report Card: This nursing home report from the State of Minnesota scores area nursing homes on seven quality measures.
Patient safety
Patient safety means focusing on reducing and eliminating accidental or preventable injuries from medical care. While Medica doesn't provide direct medical care, we can still help our providers and members reduce medical errors and keep health care safe and effective.
Medical errors are more common than many people realize. A government report published by the Institute of Medicine in 2000 found that between 44,000 and 98,000 people die each year because of medical errors in hospitals. Accidents — and near-misses — can also happen in clinics, pharmacies and other care facilities, and even at home, when patients take medicine and follow treatment orders on their own.
Information is probably the single best patient safety tool. When you talk to your doctor, your surgeon, your pharmacist or any other care provider, it's very important to ask questions and make sure you understand the answers. The Agency for Healthcare Research and Quality (AHRQ) has some helpful fact sheets to get you started (these links will take you outside the Medica site).
Medica takes part in many programs that support patient safety.
- Our Quality Resources section provides easy-to-use quality comparisons among primary care clinic systems and hospitals in the Medica network.
- Our nurses visit primary care clinics as part of our Quality Review programs. The quality review includes checks for safety features such as safe medicine storage and emergency medical equipment kept in good working order.